Breast Biopsy Methods
Are there different types of breast biopsies?
Yes, biopsies can be performed surgically (via an incision) or using various types of needles.
What is a surgical breast biopsy?
During a surgical biopsy, an entire lesion or a portion of a breast lesion is removed to examine whether the tissue contains cancer cells.
What is a needle breast biopsy?
A needle biopsy employs one of several needle types to reliably collect tissue samples or cells.
Which breast biopsy method is the most common?
Until the 1990s, surgical biopsies were used to analyze parts of breast tissue. Today, needle biopsies are preferred whenever possible.
How does the operator know where to insert the needle during a breast biopsy?
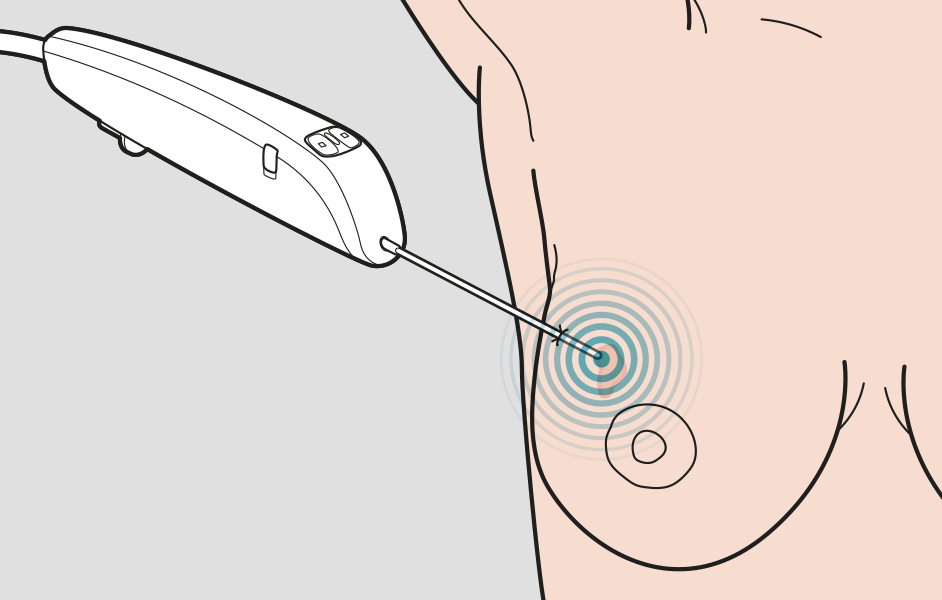
Mammography images determine the need for tissue sampling and also enable the operator to navigate the breast tissue. Biopsies often employ additional image-guidance methods. Ultrasound is the most common of these. Stereotactic biopsy or MRI-guided biopsy is used in some cases.
Ultrasound-guided breast biopsy and different types of needles
The different needle types follow slightly different naming conventions:
1. Fine Needle Aspiration (FNA)
FNA biopsy employs a very thin, hollow needle attached to a syringe to withdraw (aspirate) a small number of cells from a suspicious area.
However, using only FNA to obtain a simple cell sample (cytology) has the disadvantage of being nearly impossible to determine whether breast cancer is invasive or "in situ" (cells that resemble cancer but do not show signs of spreading). Furthermore, the information from FNA is insufficient for deciding on appropriate medical treatment.
2. Core Needle Biopsy (CNB)
The vast majority of ultrasound-guided biopsies are performed using a core needle. The CNB needle consists of two parts: an inner needle with a sharp tip and an outer sleeve that captures tissue samples when pushed over the inner needle.
Core needle biopsies have proven to be a reliable alternative to diagnostic surgery, with generally high diagnostic accuracy.
One issue with core needles, however, is their limited space for tissue collection, which can lead to uncertainty about whether the sample is representative of the lesion.
3. Vacuum-Assisted Biopsy (VAB)
Vacuum-assisted needle biopsy was developed in the 1990s to address the limitations of core needle biopsies (CNB).
Similar to CNB, vacuum-assisted needle biopsy (VAB) uses two needle sleeves. However, the outer needle is hollow with a side-notch and a solid tip. The inner needle rotates and moves into and out of the tissue, drawing it into the sample chamber with the assistance of vacuum suction.
VAB needles have a larger diameter compared to CNB and FNA, allowing them to yield more tissue. Multiple "suctions" can be performed during a single needle insertion, improving sampling results. The greater tissue yield helps reduce the likelihood of unnecessary surgeries.
The drawbacks of VAB include an increased risk of pain, bleeding during and after the biopsy, and a higher likelihood of bruising afterward.
The biopsy needle collects cells or tissue samples during the biopsy.
